Cardiomyopathy In Your Cat – When Your Pet’s Heart Fails
Ron Hines DVM PhD
The most common causes of life threatening illness in cat in North America, the UK and Europe are kidney disease (sometimes due to underlying hyperthyroidism and/or kidney disease), cancer, urinary tract blockages, inflammatory bowel disease (IBD) and diabetes – pretty much in that order. Of course, if you let your cat run loose unattended, accidents, feline leukemia and an immune system ravaged by feline immunodeficiency virus lead the list. (read here) Only one study I know of tried to tally the frequency of those causes, and that was in the UK. (you can ask me for O-Neill2015.pdf)
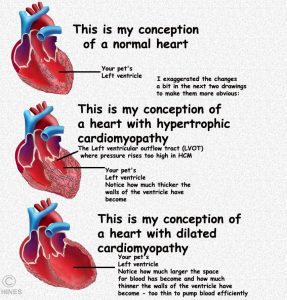
But when a cat dies quite unexpectedly, heart problems (or, occasionally heartworms in out and in-out cats) top the list. In dogs, it is diseases of the heart valves that usually lead to their heart failure. (read here) But in cats, it is disease of the heart muscle itself, cardiomyopathies, that are the most common causes. A specialized muscle (cardiac muscle) composes the four chambers of your cat’s heart. In cardiac myopathies, the muscle layer is either too thick or too thin. In whichever case, the heart looses its blood-pumping abilities. How much, depends on the severity. When severe, these problems can lead to a pet’s death.
Any cat can develop cardiomyopathies, but because this is a genetic disease, the chances are much less in random-bred (“generic”) cats because of their larger and healthier gene pool. (The chances are considerably greater in purebred cats; but because there are so many more random-bred cats than purebreds, statistics are misleading.) Veterinarians see more cases in middle-aged male cats than females [at some facilities 3:1]. Most are middle-aged by the time symptoms develop. Among the purebred cats, Maine Coon, Ragdoll, British Shorthair, Bengals, Norwegian forest, Sphinx, Chartreux and Persian cats see more of this problem that house cats originated from unplanned, random litters. Since cat breeders are more alert to the problem they are also more likely to discover these heart illnesses early in their cat’s lives than is a casual cat owner.
Not every case of heart failure in cats is due to cardiomyopathy. As in all animals and humans for a multitude of reasons, hearts sometimes just take a wrong turn in their development.
Is There More Than One Type of Cardiomyopathy?
Yes. Most folks speak about three types. But some cases mix elements of all three and a few cases defy classification beyond just saying a failing heart in a scholarly way (=“unclassified cardiomyopathies”).
Hypertrophic Cardiomyopathy (HCM)
Hypertrophic cardiomyopathy is by far the most common form of cardiomyopathy. HCM is caused by defective genetic instructions on how the heart should be built. These cats develop a heart with walls too thick (hypertrophy) and heart muscles too powerful for proper heart function. It is the left lower chamber (left ventricle 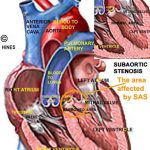
Restrictive Cardiomyopathy
Considerably less common that HCM, Restrictive cardiomyopathy (RC) is also less understood. In RC, it is the lining ( the endocardium) of the heart chambers (primarily the left ventricle) as well as the heart muscle itself that is abnormal. In this form of cardiomyopathy, scaring (fibrosis) interferes with the normal expansion and contraction of the heart chambers (The heart becomes too “stiff”) . All degrees of scaring are possible. In some cases, only limited areas of the heart are affected; in others, the entire organ. Veterinarians know considerably less about what is going wrong in these hearts than we do about cats with HCM. Restrictive cardiomyopathy occasionally occurs in all breeds of cats. As with HCM, males seem a bit more likely to develop the problem. When the restrictive form occurs, symptoms are the same in both forms. Scaring is usually associated with trauma or inflammation. But a Japanese group that examined many cats with RC thought it more likely that it occurred due to errors in cell organization and development. Although the Japanese studies found no evidence it, inbreeding (or perhaps husbandry) can play some part in its development of RV, in the only other study, all cases occurred in Cornish Rex.
Dilated Cardiomyopathy (DCM)
DCM was the most common form of cardiomyopathy in cats before 1987. It became the least common cause after it was discovered that most cases were due to a taurine deficiency. Although our bodies can synthesize taurine, your cat’s cannot. For them, it is an essential amino acid that they must obtain from their diet. Before 1987, some cat foods just didn’t have enough digestible taurine-containing protein in them to meet the cat’s needs. A taurine deficiency could still occur today in cats fed home made diets that do not contain enough high quality meat or a wacky vegan diet that utilizes soy protein without sufficient supplemental taurine. When due to a taurine deficiency and caught early, many of these problems are reversible.
In DCM, the walls of the chambers of your cat’s heart stretch become thinner and less able to pump blood efficiently. This is the opposite of what occurs in HCD and RC where the heart walls become thicker and muscle bound – but the effect on blood circulation is the same. The problem usually starts in the left ventricle, spreads to the left atrium and can eventually encompasses the entire organ. The distorted heart vales no longer work effectively and it is common for the heart’s electrical system to fail as well due to the organ’s distorted shape (eg atrial fibrillation and arrhythmias). All the potential symptoms seen in hypertrophic cardiomyopathy and restrictive cardiomyopathy can also occur as a feature of DCM. When the lack of the amino acid, taurine, was the cause, blindness (retinal degeneration) was also a quite common sign. (read here)
Veterinarians still encounter an occasion case of dilated cardiomyopathy in cats even though they are eating a taurine-rich diet. So there are apparently other factors involved. Some say that Siamese cats and breeds related to them are more prone to DCM than random bred cats. I do not know if that is true. In humans, about a third of the people that develop DCM inherited their susceptibility to it from their parents. DCM is still an important health problem in dogs. The cause of DCM in dogs is unknown; but some find taurine and carnitine supplement occasionally helpful.
What Causes Hypertrophic Cardiomyopathy?
Defective genes that govern your cat’s heart development are the underlying cause of hypertrophic cardiomyopathy. These groups of genes give instructions (direct the assembly) of the proteins that allow heart muscle to contract. These heart muscle proteins are called myosins. Like all proteins, they are composed of amino acids. When the genes that give instruction on how heart myosins should be assembled have a “typo” error, one or more of the amino acid units that form the myosin molecules is the wrong one. Many genes take part in this building processes. As of 2015, errors in 11 different genes have been linked to HCM in humans. In Main Coon and Ragdoll cats, it is the MYBPC3 gene that can be defective.
If My Cat Has Cardiomyopathy What Signs Might I See?
As I mentioned earlier, cases of cardiomyopathy range from the very mild, and imperceptible where cats act perfectly normal to very severe. In some cats, the disease progresses in severity as time goes by, in others it does not.
Lets talk about the more severe cases: There are two underlying problems that account for all the possible signs. The first is the inability of the failing heart to move blood adequately and the second is the generation of blood clots.
Cats with failing hearts lack energy. They breath faster and with more effort (dyspnea) to obtain adequate oxygen and because sluggish blood flow allows fluid to build up in their lungs (pulmonary edema). In some, fluid pools in their tummies as well (ascites). Not feeling their old selves, the cats may become very picky eaters and loose weight. Their thinness might not be obvious to owners due to the pot belly of pooled abdominal fluid, but if you run your fingers over their spine, they are often quite bony. Their pulse is often rapid. You might suspect otherwise, but It is rare for these problems to cause a cough.
Paralysis
Sluggish blood flow within the heart sometimes allows blood clots to form. Fragments of those heart clots (=thrombus/embolism) can break loose, travel down the cat’s aorta, lodge, and prevent blood flow to portions of the body. A common place for that obstruction is at the point where the cat’s main artery, the aorta, divides (the “saddle”) to supply blood to both hind legs (aortic thromboembolism= saddle thrombus= feline aortic thromboembolism= FATE) [on rarer occasions, the block lodges where the aorta branches to supply blood to the kidneys or right front leg] . Cats with blocked hind leg circulation have difficulty using those legs that ranges from a wobbly gait to complete rear leg paralysis. They are in varying degrees of hind leg pain; in fact, occasionally, pain is the only symptom. Due to reduced leg circulation, their feet and thighs may be cold to the touch. The size and exact location of these clots is unpredictable. So both legs might be effected or each to a different degree (less commonly the right front leg) As in human stroke embolisms, the problem may pass or improve on its own with time. But those cats are at very high risk of developing the problem again. When these clots do not self-correct quickly, all tissue past the clot is robed of oxygen (hypoxia) and soon dies. The preferred medication to help dissolve these blood clots and prevent their reoccurance is clopidogrel (Plavix®). However the drug is extremely bitter. Some veterinarians and cat owners have found ways to place the cats dose in empty gelatin capsules without contaminating the outside of the capsule making administration more successful.
I want to emphasize that not every case of saddle thrombus is related to an underlying heart problem – in my experience, perhaps 80% are. Lymphoma cancer that has metastasized (migrated) the cat’s spine is said to be the second most common cause of posterior and rear leg paralysis in cats. (read here) Other things can also cause aortic blockages. Problems such as hyperthyroidism or subsequent to a traumatic accident. Another point is that not every cat with cardiomyopathy will develop clot blockages. Perhaps half will. But it is easy to miss the subtle signs of a cat’s heart problems. Since it is a lot harder to miss leg paralysis, about three quarters of the cats – later found to have underlying HCM – were taken to their vet hospital because the owner noticed the paralysis – not because of suspicion of heart issues.
Why Are Cats With Cardiomyopathy More Susceptible To Blood Clots?
Traditionally, veterinarians would answer you that clots tend to form when blood moves slower than it should through the heart. Others would mention undue turbulence of blood passing through a heart that no longer retained streamlined passages designed for easy flow. Others would mention that disturbances in the pumping sequence (arrhythmias) give the heart (and the blood within it) a jerky irregular sloshy motion that makes clotting more likely to occur. That is all probably true.
Perceptive veterinary cardiologists noticed as they peered within these cardiomyopathy hearts with echocardiology visualization systems , that the blood within the upper left heart chamber (LA=left atrium) sometimes had a certain “smoky appearance” – that is now thought to be the first indications the blood might be inclined to clot (hypercoagulability). Clotting of blood is a tremendously complex process. But among the many simultaneous processes that occur, your cat’s blood clots when the platelets, distributed through out its blood become activated. Other studies suggest that stored clot activation compounds (ADP) that are stored within those platelets are somehow liberated by the processes going on in the cardiomyopathy heart. Perhaps compounds released by the specialized cells that line the heart or the failing cardiac muscle cells themselves trigger this clotting (=coagulation) cascade.
What’s Going On In My Cat’s Heart?
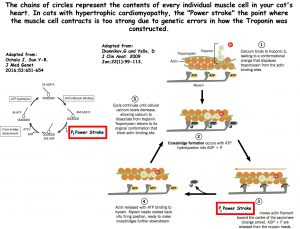
I mentioned earlier that veterinarians believe that the underlying cause of hypertrophic cardiomyopathy (and perhaps the other cardiomyopathies as well) is a genetic defect in genes that direct how the heart muscle is constructed.
The muscles of your cat’s heart are arranged in wide, spiral or helical patterns that work together to give the heart maximum torque when it contracts (a corkscrew motion also called Left Ventricular Rotation and Twist). That makes the heart the most efficient pump it can be for its size and weight so that it can eject blood with maximum force.
Between contractions (heart beat=systole) it relaxes and unwinds (=diastole). Each muscle fiber contracts in systole due to characteristic of the troponin and myosin proteins each muscle cell contains (=tropomyosin). Due to these two proteins, when calcium in the cell rise the muscle cells contract, when calcium level falls, they relax. How your cat’s troponins are constructed are under the direction of genes, such as the MYBPC3 gene found defective in some Main Coon and Ragdoll cats. That gene that was found to be sending defective instructions in Maine Coon and Ragdoll cats.
In 2016, a group of Japanese research veterinarians confirmed that in cats with hypertrophic cardiomyopathy, the twisting force (=”Power stroke”=”torsional deformation”) of heart contraction in cats with symptoms of HCM and even those genetically predisposed to HCM (but asymptomatic=no visible signs) is greater than it should be (click on the image above). That knowledge should be of great value to veterinary cardiologists in judging the severity of HCM and its potential to affect cats that currently have no symptoms but carry the genetic defect for the disease. New knowledge leads to new treatments. Not enough resources exist today in veterinary research to explore how one might decrease the intensity of this power stroke – the force that is damaging the hearts of cats that carry the mutant MYBPC3 gene or other mutant genes with the same potential. But I told you that humans also get HCM; and physicians had no better ways of slowing the progression of disease in people than veterinarians did in cats. So a company called MyoKardia in San Francisco got to work on it. Up to now, veterinarians and physicians only had drugs that increase the force of heart muscle contractions (=positive ionotropes) – drugs like digoxin and pimobendan (Vetmedin®). What they needed was a negative ionotrope, a drug that would lessen the force of heart muscle contractions. For that, they used a mouse that had been bioengineered to also develop HCM. They found one, MYK-461. They have another, MYK-491, that may be helpful in dilated cardiomyopathy where increased heart contraction force is the goal.
MYK-461 (Mavacamten) is undergoing human clinical trials. (read here) However, The MyoKardia company already provided some MYK-461 to the School of Veterinary Medicine at the University of California to try in HCM cats. Initial trials in HCM cats are said to show promise. You can read about that medication through the link at the top of this page or here.
Is It Just The Left Side Of My Cat’s Heart That Is Affected?
Not always.
When either of the three forms of cardiomyopathy occur, it is usually the left lower chamber, the left ventricle, that experiences problems first. But the defective genes that affect the force of heart muscle contraction in the left ventricle are the same genes that affect the right ventricle. So eventually, in cats, the right ventricle muscles often thicken as well increasing the pressure of blood moving to the lungs. Some veterinarians believe that
That situation could be one of the reasons many cats with HCM leak fluid from their lungs and into their chest (a plural effusion). The other common cause of plural effusions in cat is the “wet” form of FIP, feline infectious peritonitis a disease caused by a mutant feline coronavirus.
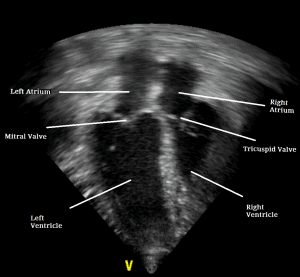
What About Cats That Have Cardiomyopathy But Show No Symptoms?
Veterinary cardiologists, using two dimensional (2D) echocardiography, can identify these cats by measuring the thickness of your cat’s left ventricular wall as well as the volume of blood it is able to eject (the difference between the full volume cavity and the empty volume cavity is less when the heart walls are thickened). The presence or absence of a heart murmur is a considerably less accurate way of detecting cardiomyopathy in its early stages (only about 1/3 of the HCM cats have them). Along with genetic testing, echocardiography is a good screening test for potential breeders. If high blood pressure can be already be well documented in these early or mild cases, I would probably begin them on one of the ACE inhibitors mentioned below – but that’s just my opinion. A beta- blocker perhaps if the echocardiographer saw evidence of marked blood turbulence or “smoke”. A T-4 test as well to be sure underlying hyperthyroidism was not a contributing cause for high blood pressure would be appropriate.
How Will My Veterinarian Diagnose This Heart Problem?
The cat’s rapid respiration, weak and rapid pulse (tachycardia),“muddy” colored gums and slowed capillary refill time (CRT) might make her/him suspicious of a heart problem. Abnormal heart sounds (arrhythmias), picked up with a stethoscope or EKG would add to those suspicions. Heart murmurs and abnormal lung sounds (moist rales) , heard through the stethoscope, would substantially reinforce that suspicion. Your explanation of the cat’s history would allow the vet to discount some other possibilities such as heat stroke, poisons, trauma, vaccine or allergic reactions.
At this point, most vets would suggest a chest X-ray. Some would run an EKG as well. In these severe cases, the heart shadow on the x-ray will be enlarged and there is usually excess fluid in the lungs. If there is still any doubt, the vet might suggest that a proBNP test be run. The proBNP test has a lot of false positives, but normal proBNP levels rarely occur in cardiomyopathy cats.
But the best test to confirm all cases of cardiomyopathy (the “gold standard”) is an echocardiogram as seen in the photo above (A heart ultrasound exam). Front line veterinarians, like myself, with general diagnostic skills, are not as adept at recognizing the telltale signs of cardiomyopathies that are apparent to veterinary cardiologists who use these machines day in and day out. Those folks are generally located in veterinary specialist centers and university teaching hospitals. Those images should show the characteristic thickened left ventricular heart walls and smaller maximum blood volume when hypertrophic cardiomyopathy is present. Looking higher up, into the left atrium, they might even detect the blood clots (=thrombi) I mentioned earlier. Elevated blood pressure due to kidney disease and or hyperthyroidism can cause similar changes. So your vet will want to rule those things out. A chest x-ray might be appropriate if lung sounds or difficulty breathing indicate that fluid may be pooling in the cat’s chest and an EKG would confirm if the heart’s rhythm is abnormal.
If you are just worried that your cat might have a genetic tendency to develop cardiomyopathies because of its breed or because parents or siblings developed the problem your vet might suggest genetic testing. At the moment, that test is available only for Maine Coon and Ragdoll cats. Two other blood test, the ProANP and ProBNP blood tests (proBNP = Antech #T1010, Idexx#2666), might also be helpful as a screening tools (proBNP false-positives do occur; false negatives are much less likely).
Can More Sophisticated Genetic Tests For HCM Be Run On My Cat And Where?
Yes, but so far the genetic defects responsible have only been worked out in certain breeds (Maine coon & ragdolls).
In the United States, the veterinary teaching hospital at North Carolina State University has the most extensive programs on cat and dog genetics and their links to disease. Their genetics lab has many studies in progress and also offers a pet genetic testing service to the public. My cardiology department at Texas A&M tells me that NC is the only lab in the USA performing these tests. In the UK, I am old that these tests are offered by Langford Vets in Bristol, in Europe, Labogen in Bad Kissingen, Germany performs these tests and, as does Antagene, La tour de Salvagny, France. They have pickup stations around the world. In Australia, Orivet in St Kilda/Melbourne conducts these tests.
A positive test result means that a cat is more susceptible to HCM than a cat that does not carry these defective genes. However the DNA test does not predict the age at which clinical onset might occur in your cat or how severe the disease might become. There is some evidence that carrier males might get the disease at an earlier age and perhaps have a more severe form.
What Medications Are Available To Treat My Cat?
You can read in detail about the pluses and minuses of these medications and others that veterinarians use to treat cardiomyopathy in cats. (ask me for Gordon2015.pdf . But as you do, please understand that most of these decisions, other than diuretics like furosemide and ACE inhibitors like enalapril are based what might help a human with HCM and that even drug plans for humans are based more on hope than on controlled studies that prove their effectiveness. In reality, survival time in 2017 is not much different than it was 25 years ago when these newer medications were unknown.
Veterinarians have no means of reversing the damage caused to cats by cardiomyopathy. The best we can hope for is to perhaps slow the progress of the disease and make a cat’s life as comfortable as possible. Perhaps, drugs like MK-461 or other breakthroughs will offer hope in the future.
But for now, veterinarians concentrate on prescribing medications that help stabilize your cat’ heart rate (beta blockers), medications like ACE inhibitors that improve blood circulation, administering diuretics if pooled chest fluids are making the cat’s breathing difficult and administering medications that make blood clots less likely.
Furosemide (Lasix®)
Diuretics like furosemide are some of the mainstays for treating many forms of heart failure (CHF=congestive heart failure) in people and pets. Congestive means that in those forms of heart problems fluid is leaking out of blood vessels and into the surrounding tissue (edema) and furosemide does an excellent job at allowing the kidneys to flush some of that excess water (and sodium) into the urine. That action “dries” out their excessively “wet” lungs and allows cats with HCM to breath more easily. The required dose in cats is highly variable. One tries to use the minimum dose at the widest spacing (interval) that will keep the cat breathing comfortably. As time goes by, that dose will increase. At high doses, the cat’s potassium levels sometimes become too low. In those cases, vets often add another diuretic, spironolactone, that allows the furosemide dose to be lower.
Spironolactone (Aldactone®)
Spironolactone is also a diuretic. Particularly high doses of furosemide sometimes lead to too much potassium loss through the cat’s kidneys (=hypokalemia). When that occurs, adding spironolactone as a second diuretic that does its work in a different manner often allows the furosemide dose given to your cat to be lowered to a safer level.
ACE Inhibitors (enalapril , benazepril, ramipril, etc)
If your cat has progressed to the point where it needs diuretics like furosemide, it probably needs an ACE inhibitor as well. Ace inhibitors lessen the hearts’ effort needed to move blood throughout the circulatory system by relaxing (dilating) the special muscles fibers within the walls of the cat’s blood vessels throughout its body. These drugs might offer some protection for your cat’s kidneys as well. ( read here & here)
Atenolol (Tenormin®)
Atenolol is a beta blocker medication. One of a group that have traditionally been used to lessen heart arrhythmias (abnormally timed heart beats) in humans. It is occasionally given to cats with HCM in an attempt to lessen these abnormal heart beats – particularly when they occur in the left upper heart chamber where arrhythmias (atrial fibrillation) and blood turbulence are thought to encourage the formation of blood clots. It is also thought that the drug might have some positive effects when the heart distortions of HCM obstruct the easy flow of blood out of the left side of the heart on its way to the rest of the body (LVOT obstructions= the left ventricular outflow tract). A heart, like a motorcar engine, must be in perfect timing in its power stroke as to when valves open and close. However, drugs that should work, in theory, sometimes don’t work in fact. Such may be the case with atenolol but that is still uncertain. Some vets use a somewhat similar medication, Sotalol, in an attempt to lessen those arrhythmias.
Calcium Channel Blockers
Calcium channel blockers are medications that also lower blood pressure. One research veterinarian reported that one of those medications, diltiazem, slowed the progress of HCM in cats. (read here) However the side effects, dosing challenges and a failure to obtain the positive results the authors reported make its use rare today.
Pimobendan (Vetmedin®)
Pimobendan increases the force of your cat’s heart contractions (drugs that do that are called positive ionotropes). That is important in dogs and humans where the dilative form of cardiomyopathy is common and the heart muscle walls expand, thin, and become weak or in congestive heart failure brought on by heart valve disease – uses for which it is FDA approved. But neither is common in cats. Most vets reserve this drug for the very late stages of HCM when the cat is on a rapid, downward health trajectory in an attempt to salvage a little more time for the creature.
Pain
When cats are presented with blood clots that lodge in their aorta (=feline aortic thromboembolism = saddle thrombus = FATE = ATE); they require narcotic pain medication for 24-48 hours. (read here) After that, pain-control decisions have to be made on a case-by-case basis. In an attempt to dissolve the clots, some veterinarians use dalteparin sodium (Fragmin®) others clopidogrel (Plavix®) and a few, still give aspirin. You can read general approaches veterinarians use to control pain in cats here.
How Will I Know If These Medications Are Helping My Cat?
Most cats with cardiomyopathy are brought to veterinarians either because owners noticed that their pet is breathing faster than normal or because of hind leg weakness or hind leg paralysis. Resting breathing rate in cats is quite variable; but normal cats take less than 30 breaths per minute. If your cat’s respiratory rate falls into the normal range after a week on its medications, that is a very good sign. When paralysis and leg weakness were the issues, more mobility and less apparent pain are what veterinarians are looking for and what owners should be too.
There are many other, more subtle signs that cat owners can look for to judge if their pet’s current medication plan is helping. Veterinarians at Tufts Veterinary School designed a questionnaire to guide you through that assessment. They call it their CATCH questionnaire and they find it helpful in adjusting medication doses and medication choices.
Frequent repeat laboratory tests, like NT-proBNP and echocardiographic parameters (results) are no better in judging a cat’s positive or negative response to medications than is a perceptive owner’s feedback. Besides, frequent pet hospital visits involve stress and possible anesthetic and restraint requirements that can make matters worse (= decompensate a clinically stable cat).
Collapse, increased exercise intolerance (weakness & lethargy) , a new or worsening cough, decreased appetite, the worsening of paralysis or pain are all reasons to immediately contact your veterinarian.
Corticosteroid medications (eg prednisolone, methylprednisolone, prednisone etc.), given orally or by injection, are best avoided in cats with all types of heart problems. That class of medication encourages fluid buildup in the body. Major life changes such as the introduction of new cats and lifestyle changes are also best avoided. When you travel, never board cats with heart or other serious health issues. The stress of unfamiliar settings is too great. Instead, hire an experienced pet sitter who comes to your home. A stay at a “pet resort” is never a happy experience for a cat.
How Much Longer Might My Cat Live?
When hypertrophic cardiomyopathy was picked up on an echocardiographic screening test and not because of heart symptoms they can survive for years and, perhaps, lead a long normal life. Many of those cats were sent to a cardiology specialist because their primary vet detected a heart murmur. Some veterinarians also recognize a “focal” form of HCM in which only isolated portions of the heart muscle appear affected and overall heart function remains adequate.
But when the diagnosis was made because of symptoms, the prognosis for an extended life is not nearly as bright. The Cornell Feline Health Center’s cardiologists consider an additional year of life optimistic for cats that are already showing significant symptoms of HCM. The vets at the Royal Veterinary College in the UK did the most through study regarding how long cats that had been diagnosed with HCM might live. For two years, they followed 255 cats in which a HCM diagnosis had been made. At the end of 2 years, 55.3% percent of the cats were still alive. Of the ones that were no longer alive, 9% had died from the results of blood clots, 17.3% had died from congestive heart failure (CHF), 4.7% had just died unexpectedly. The other missing cats had died from causes unrelated to their heart problems or been euthanized because of them. Cats that were already showing signs of heart failure and those which showed the most severe heart wall thickening (=“reduced left ventricular fractional shortening”) were the least likely to have survived.
In an earlier study, the same group of veterinarians found that when echocardiograms showed that the cat’s left atrium was larger than normal, their period of survival was shorter. Others have found that cats whose heart rates are exceedingly fast (=tachycardia=>200 beats/min) are likely to survive only a short time.
A French group of veterinarians looking back over their data found that ordinary domestic short-hair cats, Persians and Chartreux cats tended to survive longer than other breeds after the diagnosis of HCM was made. They had no explanation for that. Breeds that did the poorest in terms of survival time were Maine Coon (~2.5 years) and Sphinx (~3.5 years). Perhaps a hint that different genetic defects – all with the ability to cause HCM – are present in different cat breeds. Ask me for Trehiou-Sechi.
Angell Memorial Hospital is the premier SPCA hospital in Boston and one of the best on the Eastern U.S. seaboard. In a 2017 website interview, they mention that the owners of HCM cats presented with blood clot paralysis (Feline Aortic Thromboembolism = FATE) are not vigorously encourage to begin medication or extreme measures to prolong their cat’s lives. Perhaps that is because they know that long term successes are scant and because they know that cats resent prolonged medication, manipulation and extreme measures. Euthanasia at the time of presentation is their most common outcome. But when owners of FATE cats elect treatment anyway, only approximately 50% of the cats survived long enough to be discharged from their hospital.
You are on the Vetspace animal health website
Visiting the products that you see displayed on this website help pay the cost of keeping these articles on the Internet.